The development of osteochondrosis of the lumbar spine is manifested by pain in the back and legs, fatigue and poor posture. The causes of this pathology can be very diverse, therefore the treatment of lumbar osteochondrosis must be carried out under the strict supervision of a doctor. In advanced cases, the disease leads to serious disabilities and the person may become disabled. Degenerative disease with this type of osteochondrosis is fixed at the level of the vertebrae L1 S1, L2-L3, L3 S1 and in the area of the L5 S1 disc.

Osteochondrosis of the lumbar spine is a dangerous disease of the musculoskeletal system that can lead to disability.
The main causes of damage to the lumbar vertebrae
Lumbar osteochondrosis arises due to the influence of such pathological factors on the body:
- uneven load on the spine;
- low physical activity, sedentary work;
- hard work associated with heavy loads;
- genetic predisposition, in which the pathology is diagnosed in childhood;
- flat feet;
- overweight;
- infectious and inflammatory diseases.
Symptoms of osteochondrosis of the lumbar spine
The degenerative process in the lower back causes sharp pain in the lower back in men and women, radiating to the leg along the location of the sciatic nerve. Signs of lumbar osteochondrosis do not manifest themselves for a long time; a feeling of discomfort and swelling occurs already at stages 2-3.In the more advanced stages of the disease, symptoms are uncomfortable with coughing, sneezing and little physical activity. The pathology also causes radicular syndrome:
- shooting, sharp pain occurs in the lower back;
- skin sensitivity on the lower extremities is impaired;
- worried about muscle weakness;
- tingling appears in the legs and knee joint;
- sweating is impaired.
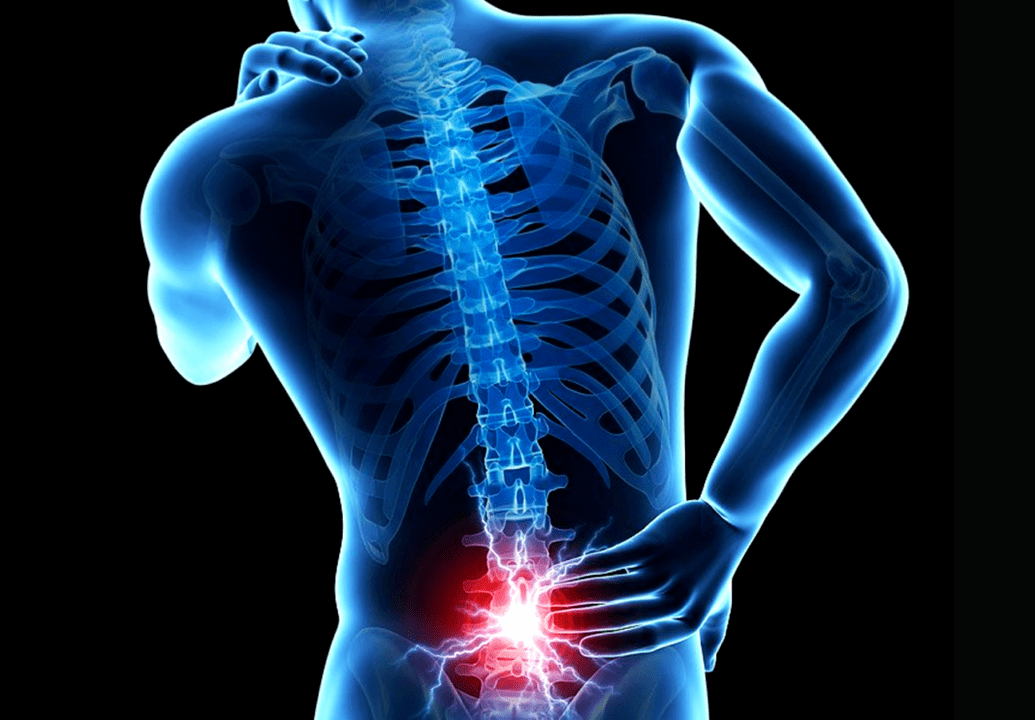
The main symptom of lumbar osteochondrosis is pain in the lower spine.
A degenerative disease involves limited mobility, difficulty trying to bend over, and pain with minimal effort. If treatment of lumbar osteochondrosis is not started in a timely manner, serious consequences arise, including deformation of the intervertebral disc, protrusion and the appearance of a hernia. These disorders can only be treated surgically, as conservative therapy does not help.
Degrees of pathology
1st degree
The inner layer of the fibrous ring becomes covered with fissures, through which the nucleus pulposus begins to emerge. As it passes outward, the nerve fibers become irritated. A person feels how his back hurts in the lower back with minimal loads. In stage 1, the pain caused by osteochondrosis is usually stable, but the low back pain can be bothersome. Symptoms disappear after rest and do not bother you for a long time.
2nd degree
When the 2nd period of the pathology begins, the intervertebral space decreases, the nerve fibers are compressed more strongly, the pain becomes intense, pseudospondylolisthesis and left-sided scoliosis develop. The fibrous ring is most actively destroyed. Populus osteochondrosis of the 2nd degree is characterized by pathological mobility of the spine. Due to the increased load, a person plays in the cold, and then in the heat. Symptoms become pronounced and cannot be ignored. The attacks become longer and longer and the pain cannot be relieved with the usual painkillers.
3rd degree
The course of third-degree osteochondrosis of the lumbar region is characterized by increased pain, deformation of the spine and reactive growth of bone tissue. The fibrous ring ruptures and the nucleus pulposus leaves its limits, causing a hernia. If treatment is not started at stage 3 of development, the patient is at risk of becoming disabled.
4th degree

Grade 4 osteochondrosis of the lumbar spine does not allow a person to walk due to severe pain.
There is complete deformation of the spine, pain in the legs and back becomes unbearable and the person is unable to move independently. If chondrosis treatment is not started at the 4th stage of development, disc protrusion occurs, which can only be treated surgically. After surgery, the patient's health is not always fully restored.
Diagnosis
When you are concerned about signs of osteochondrosis of the lumbar spine, you need to see a doctor. At the initial consultation, the doctor will palpate the coccyx, the iliac crest region, and will also determine the manifestation of the following syndromes:
- development of scoliosis, kyphosis and osteoarthritis;
- pain in specific points;
- inability to perform certain movements;
- the level of location of the gluteal folds, which can be on the right or left side.
An x-ray is performed, which takes photos of the affected area. In the image, the lumbar region appears deformed in advanced stages, with protrusions visible on the right or left; For a more detailed diagnosis, a CT or MRI scan is prescribed, thanks to which the doctor will receive the results as quickly as possible and select the optimal treatment methods.
How is the treatment carried out?

Medicines and surgery
The choice of method of treatment for osteochondrosis of the lumbar spine depends on the degree of the disease.
Chronic lumbar osteochondrosis must be treated comprehensively. This means that self-medication is unacceptable. The treatment protocol must be determined by the doctor, who will select the necessary medications with minimal side effects. The treatment regimen involves the use of:
- analgesics;
- nonsteroidal anti-inflammatory drugs;
- muscle relaxants.
First aid involves the use of injection blocks, which relieve pain, relieve swelling and the temperature of the affected area. The acute phase, in which the pain syndrome is pronounced, is treated with potent analgesics. As an auxiliary therapy, treatment with local agents is recommended - ointments, gels and creams. If conservative treatment does not help or the disease is diagnosed in advanced stages, surgical therapy is prescribed. When hernias form, they are completely removed. Then the compression of nerve fibers and blood vessels is eliminated. If necessary, the affected vertebra is removed and an implant is placed in its place.
Massage and manual therapy
A course of therapeutic massage will help reduce pain and alleviate the symptoms of lumbar osteochondrosis in women and men. Even children who suffer from the disorder undergo this therapy, but the main condition is that the procedure is carried out by a trained chiropractor who is aware of the diagnosis, otherwise complications may arise.
Back to content
Therapeutic exercises
Restorative gymnastics will help normalize blood circulation in the affected lower back and strengthen the muscles around the spine. It is important to make movements with osteochondrosis carefully, trying not to force too much. It is advisable that the first exercises are carried out under the supervision of a trainer, who, if necessary, will help to correct the movement at the right time.
Physiotherapy and acupuncture
One of the effective types of physiotherapeutic procedures is considered amplipulse, when pulses of modulated current are sent to the affected areas. Thanks to this effect it is possible to reduce inflammation, relieve swelling and reduce pain. Acupuncture has an equally pronounced effect: it relieves muscle tension, relieves symptoms and accelerates tissue regeneration.
If lumbar osteochondrosis is diagnosed, you cannot do without gentle nutrition. It is recommended to enrich the menu with products containing calcium, phosphorus, magnesium, zinc and folic acid. It is important to maintain a drinking regime and drink at least 6 tablespoons per day. water. You must give up bad habits and a sedentary lifestyle.
Dangerous consequences and their prevention
Prevention of osteochondrosis of the lumbar spine includes exercise therapy, healthy eating and giving up bad habits.
If incipient lumbar osteochondrosis is diagnosed in a timely manner, the disorder can be cured with a course of drug therapy and special exercises. Otherwise, there is a risk of developing intervertebral hernias, sciatica, osteoarthritis, paresis and other vertebral disorders that can make the patient disabled. For the treatment to be effective, it is important to consult a doctor in a timely manner. As preventive measures, it is recommended to perform spinal traction, control posture, strengthen muscles and evenly distribute the load. Additionally, you should exercise, monitor your diet, and drink at least 6 to 8 tablespoons. water per day. At the first symptoms, do not self-medicate, but go to the doctor and strictly follow the prescribed treatment regimen.



















